Asking the Right Questions: How Many Medicare Participants Are At Risk of Harm from Prescription Opioids?
Over 14 million Medicare participants received opioid prescriptions in 2016—which cost the government over $4 billion. Because of the recent increase in opioid overdoses, Medicare monitors participants that might be overutilizing opioids.
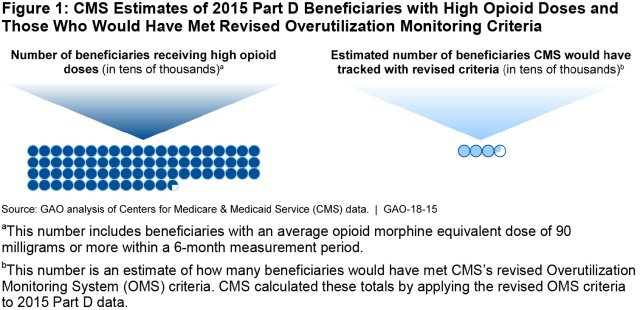
However, we found that there are more Medicare participants at risk of harm from opioids than the program monitors. Based on Centers for Disease Control and Prevention guidelines, nearly three quarters of a million Medicare participants were potentially at risk of harm from opioids in 2015—but Medicare would have only monitored about 33,000 of them.
How did GAO determine that nearly 750,000 are at risk for opioid harm?
According to CDC’s guidelines, physicians should carefully assess the benefits and risks of prescribing opioids that exceed 90 mg a day (of morphine equivalent dose) because this dosage level can lead to significant risk of overdose and death.
In 2015, Medicare estimated that 727,016 Medicare participants were prescribed an average daily dose of 90 mg or more during a 6-month period in 2015. So, according to CDCs guidelines, these 727,016 Medicare participants may have been at risk for harm from opioids. This number excludes those with a cancer diagnoses or in hospice care.
In our work, we consulted with associations that represent pain management physicians and patients. Some patients may require high opioid doses that exceed 90 mg or more for the management of their pain. Nevertheless, those individuals may still be at risk of harm. According to CDC guidelines, risks for patients aged 65 and older can be even greater. Yet Medicare does not know whether the number of patients at risk is increasing or decreasing over time.
Why is the Medicare number so much lower?
Medicare would have only monitored 33,223 of these participants in 2015 because it looks for:
- Participants that receive opioid prescriptions that are greater than 90 mg a day
AND
- Participants who receive opioids from four or more doctors and four or more pharmacies (or from six or more doctors)
Why does this matter?
It means that Medicare can’t fully keep track of whether the number of patients at risk from prescription opioid harm is increasing or decreasing over time. Medicare needs this information to see if its efforts at reducing this harm are working.
Reducing prescription opioid abuse could also lead to a cost savings for Medicare since it may decrease the number of prescriptions that are being filled inappropriately.
What should Medicare do about it?
We recommended that Medicare track the number of its participants that are receiving high doses of opioids, regardless of the number of doctors that provide those prescriptions or the number of pharmacies that fill them, so the program can tell if the overall number of people at risk of harm is increasing and decreasing.
We also recommended that Medicare identify and monitor doctors who prescribe high amounts of opioids.
How do people abuse prescription opioids?
Prescription opioids (like hydrocodone, oxycodone, and morphine) are used to treat pain and they can legitimately help people deal with chronic pain. However, they can also lead to drug dependence, overdose, and death. The CDC reported almost 4 times more deaths from prescription opioid overdoses in 2013 than in 1999.
We previously reported on some ways that people abuse and can be harmed by opioid prescriptions, including:
- “Doctor shopping”—getting multiple opioid prescriptions from different doctors or from multiple pharmacies
- Using prescription opioids recreationally, selling them on the black market, giving them to family or friends who may be trying to self-medicate, or pretending to be in pain to get a prescription.
- Questionable prescribing practices. Some doctors—commonly known as “pill mills”—write unnecessary prescriptions or prescribe larger quantities than are medically necessary.
What does Medicare do when it finds potential abuse?
Medicare generates quarterly reports of participants who meet its criteria for high risk for prescription opioid abuse and distributes these reports to the private organizations (e.g., health insurance companies) that implement its drug benefit program. These organizations must then take steps to curb potential abuse and inform Medicare of the steps they took to do so. These steps could include:
- Letting doctors know when a participant is receiving high levels of opioids from other doctors
- Restricting some participants to certain amounts and certain opioids. Pharmacists would receive a message when a Medicare participant attempts to fill a prescription that exceeds their limit.
- Investigating whether a Medicare participant is using their prescription opioids recreationally or selling them on the black market
- Potentially restricting certain Medicare participants to a single pharmacy for all their opioid prescriptions (beginning in 2019)
For more information, check out our full report.
- Comments on GAO’s WatchBlog? Contact blog@gao.gov.
GAO Contacts
Related Products

GAO's mission is to provide Congress with fact-based, nonpartisan information that can help improve federal government performance and ensure accountability for the benefit of the American people. GAO launched its WatchBlog in January, 2014, as part of its continuing effort to reach its audiences—Congress and the American people—where they are currently looking for information.
The blog format allows GAO to provide a little more context about its work than it can offer on its other social media platforms. Posts will tie GAO work to current events and the news; show how GAO’s work is affecting agencies or legislation; highlight reports, testimonies, and issue areas where GAO does work; and provide information about GAO itself, among other things.
Please send any feedback on GAO's WatchBlog to blog@gao.gov.