VA’s Response to Veterans’ Increasing Demand for Mental Health Services
May is Mental Health Awareness month. The COVID-19 pandemic has taken a toll on the mental health of individuals in the U.S. But, even before the pandemic, mental health was a long-term and growing concern for veterans. Our analysis of federal health policy includes work focused on the mental health needs of veterans—including, how the Department of Veterans Affairs (VA) can improve its mental health services and decrease veteran suicides, which occur at a higher rate than for the general population.
In today’s WatchBlog post, we look at a series of reports about the increasing demand for VA’s mental health services, and how VA is responding to this demand.
What risks and barriers do veterans face related to mental health?
In addition to combat-related trauma, such as post-traumatic stress disorder, which may increase the risk of mental health conditions, certain populations of veterans may experience additional risks and barriers. For example:
- Sexual trauma experienced by individuals in the military can lead to depression and anxiety among veterans.
- Mental health provider shortages may mean veterans living in rural areas have less access to mental health services.
- Homeless veterans with mental illness may experience additional barriers to accessing housing and employment services designed for the general population.
What can VA do to improve the mental health services it provides to veterans?
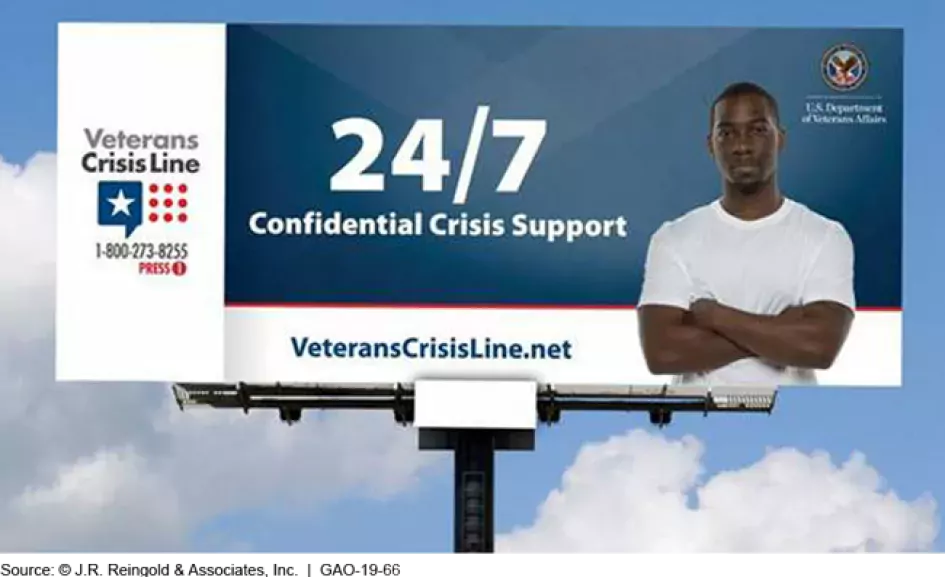
VA operates one of the largest health care systems in the country, and one-third of its veteran patient population has one or more mental health conditions. Yet, we found that some veterans may be unaware of the services and benefits available to them. Our work has pointed to the importance of outreach efforts to raise veterans’ awareness of VA’s mental health services and suicide prevention resources, such as the Veterans Crisis Line. The Veterans Crisis Line is a national toll-free hotline that supports veterans in emotional crisis.
Image
We also found that data VA collects about its veteran population may be inconsistent or incomplete. We recommended that VA improve its data collection for race and ethnicity, and sexual orientation and gender identity, which could help to better assess whether its efforts are improving mental health outcomes for veterans.
To learn more about how VA can improve the mental health services it provides to veterans, check out our latest Health Care Capsule—a new product designed to summarize multiple GAO products on related issues—on Veterans’ Growing Demand for Mental Health Services.
And tune into our podcast with GAO’s Debra Draper about VA’s Suicide Prevention Program, and find out whether this program is offering veterans the support they need.
- Comments on GAO’s WatchBlog? Contact blog@gao.gov.





