Science & Tech Spotlight: Herd Immunity For COVID-19
Fast Facts
“Herd immunity” can happen once a large part of a population—say 70-90%—develops immunity to a disease. This generally happens by infection (conferring natural immunity) or vaccination. Herd immunity can help slow or stop a disease’s spread, but many people may die before it happens.
It is currently unclear how herd immunity could happen for COVID-19. For example, the data are insufficient to show how much immunity infection confers, or whether it’s enough to prevent re-infection. How long any immunity will last is also unknown. Related viruses confer some immunity after infection, but that immunity doesn’t seem to last longer than a year.
Herd immunity can help slow or stop the spread of a disease
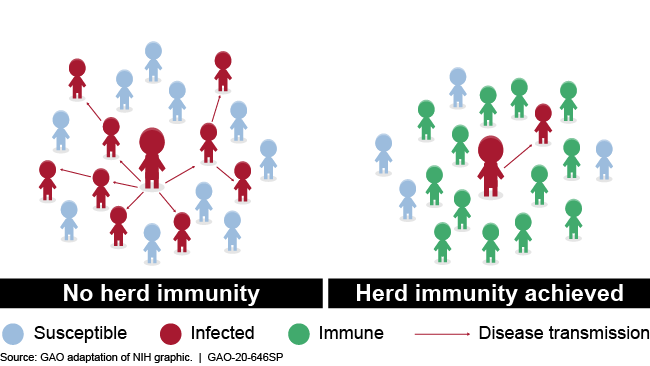
Illustration showing transmission with and without herd immunity
Highlights
Why This Matters
Increasing the immunity of a population to an infectious disease like COVID-19 can slow the spread of infection and protect those most vulnerable. However, with limited information about important aspects of COVID-19, there are challenges to understanding the implications of herd immunity in the current pandemic.
The Science
What is it? A population can establish herd immunity to an infectious disease once a large enough portion of the population—typically 70 to 90 percent—develops immunity. Reaching this "herd immunity threshold" limits the likelihood that a non-immune person will be infected. In general, immunity develops through either infection (resulting in natural immunity) or vaccination (resulting in vaccine-induced immunity). Herd immunity helps protect people not immune to a disease by reducing their chances of interacting with an infected individual. This process slows or stops the spread of the disease.
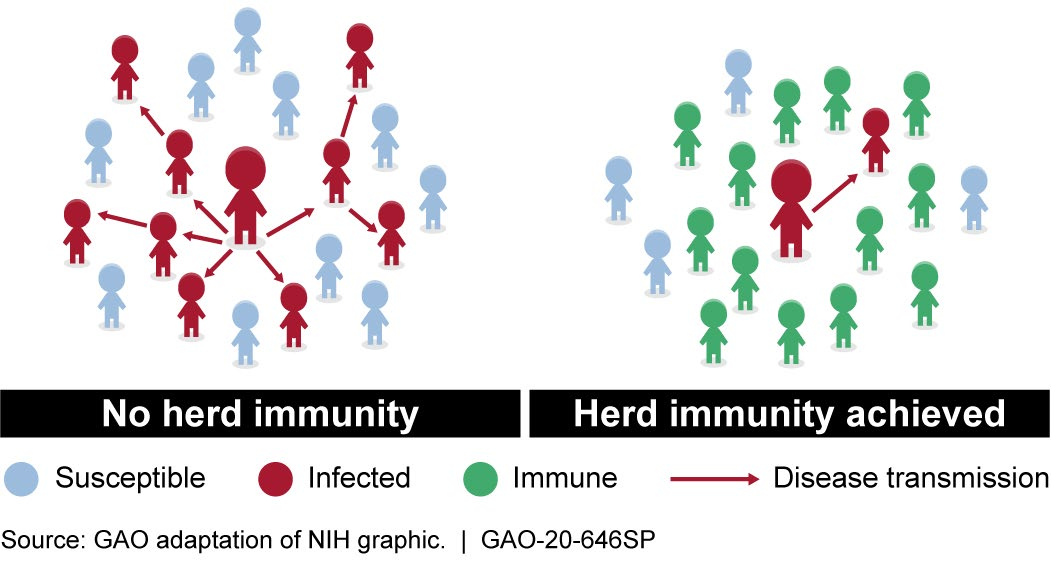 Figure 1. Herd immunity helps reduce the likelihood of disease transmission from infected individuals to non-immune individuals.
Figure 1. Herd immunity helps reduce the likelihood of disease transmission from infected individuals to non-immune individuals.
How does it work? Once a community has established herd immunity, someone without immunity is less likely to be exposed to an infectious individual during an outbreak. For example, because there are more people with immunity in the population, there are fewer people susceptible to infection, and thus the number of potential transmissions is limited. Similarly, those who are immune will not be infected, and thus will not transmit the disease to others. Both of these situations help limit the size of the outbreak.
If an effective vaccine is available for a virus, achieving herd immunity can require a high rate of vaccination in the community. For diseases that spread more easily, more people must have vaccine-induced or natural immunity to achieve herd immunity. However, if a virus mutates quickly, the community's herd immunity may be relatively short-lived because the immunity from prior infection or vaccination may no longer be effective. Also, the disease can still circulate in segments of the population that are not immune, such as those with weakened immune systems who cannot effectively form immunity.
For diseases where no vaccination is available, it is possible to develop herd immunity through exposure to, and recovery from, the disease. However, if COVID-19 runs its natural course, this approach would entail the risk of severe disease or death. Given the risk associated with COVID-19 infections, achieving herd immunity without a vaccine could result in significant morbidity and mortality rates.
How mature is it? Knowledge of previous infectious disease outbreaks where a vaccine was available has allowed researchers to identify how herd immunity was achieved for those diseases. However, researchers currently have insufficient data on the factors that could contribute to herd immunity for the COVID-19 pandemic. These factors include the herd immunity threshold, the number of secondary cases typically generated by an infected individual, the viral mutation rate, and the length of time immunity lasts.
At this stage in the COVID-19 pandemic, researchers have insufficient data to draw definitive conclusions about the level of immunity conferred by an infection, or how long immunity to the disease might last. For example, in order to determine the herd immunity threshold, it is important to know how contagious the disease is–which is affected by factors such as how many susceptible people an infected person can infect. While researchers have developed estimates for how contagious COVID-19 is, uncertainties about case reporting and testing—such as uncertainty in the accuracy of some tests—make this calculation difficult. Some peer-reviewed research on COVID-19 suggests the average number of people infected by a contagious person ranges from about one to seven.
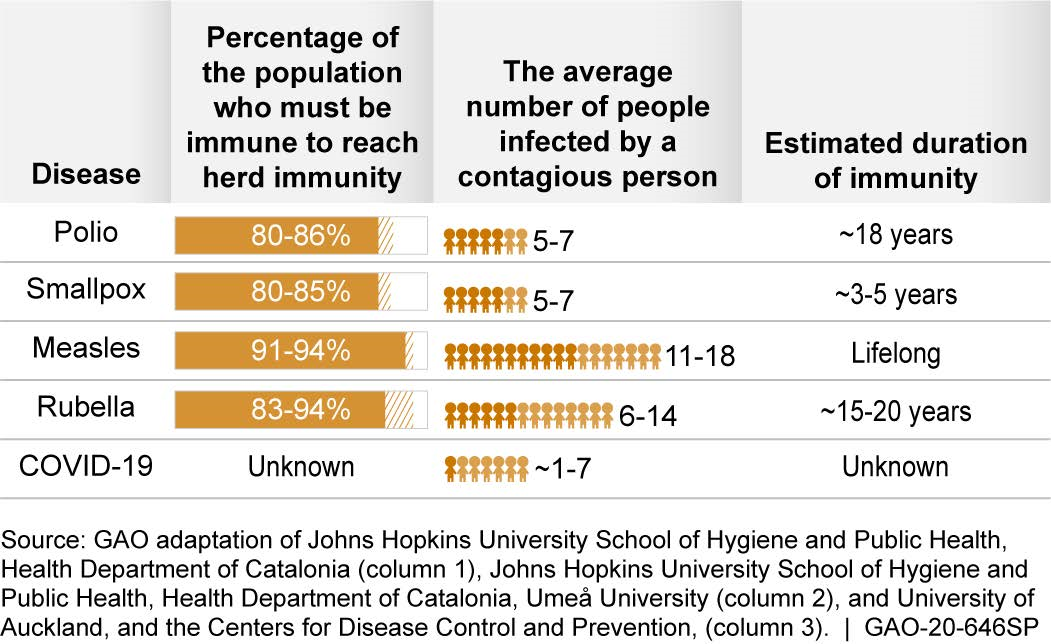
Figure 2. While data on previous disease outbreaks are available, for COVID-19, we don’t yet have all of the necessary data for many of the relevant factors.
While analyses of viruses related to the novel coronavirus have shown that infection can provide some level of immunity, such immunity did not appear to last longer than a year. Studies of other infectious diseases, such as polio, exhibit a range in the threshold for herd immunity, the average number of people infected by an infected person, and how long people remained immune, among other factors.
Opportunities
- Halt disease spread. Achieving herd immunity will slow or stop the spread of a disease within a population and limit the size of outbreaks.
- Support economic recovery. Established herd immunity could help bolster the economy by allowing people to safely return to work and conduct other activities.
- Restore medical capacity. Established herd immunity could help ease the burden on the medical system as fewer patients seek treatment.
Challenges
- Limited data on immunity. Currently, there are a number of unknown factors, such as whether a COVID-19 infection leads to immunity and how long immunity might last. It may be necessary for more time to pass to monitor individuals who have been infected and recovered and thus determine how long they show disease immunity. This information is needed to determine the herd immunity threshold.
- Implications of natural herd immunity. Relying on natural immunity from the disease progression of COVID-19 could allow a population to establish herd immunity. However, such an approach risks exposing people to a debilitating and potentially fatal disease.
- Testing limitations. If infection confers immunity, researchers need accurate data on the number of recovered individuals and other disease transmission parameters to determine if or when herd immunity is achieved. Accurate testing data are critical to understanding these parameters. However, there are still challenges associated with the use and availability of antibody tests, as well as with determining their accuracy.
- Lack of vaccine. A vaccine could help a population safely achieve herd immunity. However, developing a vaccine is a complicated process that is costly, typically requires 10 to 15 years or more, and many candidates fail during the development process. Efforts are underway, however, to accelerate the process for COVID-19.
- Inconsistent immunity. Even if herd immunity is eventually achieved, outbreaks may still occur because immunity may not be uniform across the general population.
Policy Context and Questions
- What studies are needed to gather data on the parameters for herd immunity against COVID-19, and how can this be reflected in resource priorities?
- If a COVID-19 vaccine is approved but the number of available doses is still limited, what factors may need to be considered in deciding who should be vaccinated first?
- If the path to COVID-19 herd immunity is uncertain, what steps might be needed to help strike a balance between public health and enabling the economy and society to function smoothly?
- How could infectious disease modeling assist in working towards establishing herd immunity?
For more information, contact Karen Howard at (202) 512-6888 or HowardK@gao.gov.
