Nursing Home Quality: CMS Should Continue to Improve Data and Oversight
Highlights
What GAO Found
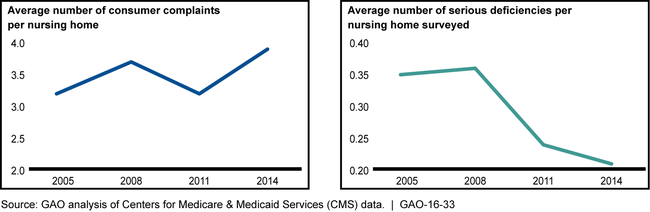
In recent years, trends in four key sets of data that give insight into nursing home quality show mixed results, and data issues complicate the ability to assess quality trends. Nationally, one of the four data sets—consumer complaints—suggests that consumers' concerns over quality have increased, while the other three data sets—deficiencies, staffing levels, and clinical quality measures—indicate potential improvement in nursing home quality. For example, the average number of consumer complaints reported per home increased by 21 percent from 2005-2014, indicating a potential decrease in quality. Conversely, the number of serious deficiencies identified per home with an on-site survey, referred to as a standard survey, decreased by 41 percent over the same period, indicating potential improvement. The Centers for Medicare & Medicaid Services' (CMS) ability to use available data to assess nursing home quality is complicated by various issues with these data, which make it difficult to determine whether observed trends reflect actual changes in quality, data issues, or both. For example, clinical quality measures use data that are self-reported by nursing homes, and while CMS has begun auditing the self-reported data, it does not have clear plans to continue. Federal internal control standards require agencies to monitor performance data to assess the quality of performance over time.
Consumer Complaints and Serious Deficiencies, 2005 - 2014
In recent years, CMS has made numerous modifications to its nursing home oversight activities, but has not monitored the potential effect of these modifications on nursing home quality oversight. Some of the modifications have expanded or added new oversight activities, while others have reduced existing oversight activities. According to CMS, some of the reductions to oversight activities are in response to an increase in oversight responsibilities and limited number of staff and financial resources. However, CMS has not monitored how the modifications might affect CMS's ability to assess nursing home quality. For example, CMS reduced the number of nursing homes participating in the Special Focus Facility program—which provides additional oversight of homes with a history of poor performance—from 152 in 2013 to 62 in 2014. State survey agency officials who conduct surveys for CMS also made modifications which could have either a positive or negative effect on oversight, but CMS does not have an effective mechanism for monitoring. Federal internal control standards require ongoing monitoring as a part of normal program operations; without this monitoring, CMS cannot ensure that any modifications in oversight do not adversely affect its ability to assess nursing home quality.
Why GAO Did This Study
To help ensure nursing home residents receive quality care, CMS, an agency within the Department of Health and Human Services (HHS), defines quality standards homes must meet to participate in the Medicare and Medicaid programs. To monitor compliance with these standards, CMS enters into agreements with state survey agencies to conduct on-site surveys of the state's homes and also collects other data on nursing home quality. CMS and others have reported some potential improvements in nursing home quality.
GAO was asked to study these trends. This report examines (1) the extent to which reported nursing home quality has changed in recent years and the factors that may have affected any observed changes, and (2) how CMS oversight activities have changed in recent years. GAO analyzed four sets of CMS quality data—deficiencies cited on standard surveys (2005-2014), consumer complaints (2005-2014), staffing levels (2009-2014), and a sub-set of clinical quality measures (2011-2014)—at both national and state levels. We also reviewed relevant documents, including CMS guidance and Standards for Internal Control in the Federal Government, and interviewed CMS and state agency officials at 5 states selected on factors such as size.
Recommendations
GAO recommends, among other things, that CMS implement a clear plan for ongoing auditing of self-reported data and establish a process for monitoring oversight modifications to better assess their effects. HHS agreed with GAO's recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | To improve the measurement of nursing home quality, the Administrator of CMS should establish specific timeframes, including milestones to track progress, for the development and implementation of a standardized survey methodology across all states. |
HHS concurred with this recommendation, established timeframes and milestones, and, in November 2017, finalized and made the standardized survey methodology effective in all states.
|
| Centers for Medicare & Medicaid Services | To improve the measurement of nursing home quality, the Administrator of CMS should establish and implement a clear plan for ongoing auditing to ensure reliability of data self-reported by nursing homes, including payroll-based staffing data and data used to calculate clinical quality measures. |
HHS concurred with this recommendation and provided evidence of auditing processes for both the payroll-based staffing data and the data used to calculate clinical quality measures. Specifically, for the payroll-based staffing data CMS provided documentation that it started ongoing audits of the accuracy of the staffing data in 2018. For the data used to calculate clinical quality measures, CMS provided documentation in 2019 that the data can be audited for accuracy through a revised survey process.
|
| Centers for Medicare & Medicaid Services | To help ensure modifications of CMS's oversight activities do not adversely affect the agency's ability to assess nursing home quality and that effective modifications are adopted more widely, the Administrator of CMS should establish a process for monitoring modifications of essential oversight activities made at the CMS central office, CMS regional office, and state survey agency levels to better understand the effects on nursing home quality oversight. |
HHS concurred with this recommendation and provided evidence in 2020 of monitoring modifications of oversight activities such as reviewing the effect of federal monitoring survey changes.
|
