Medicaid: Additional CMS Data and Oversight Needed to Help Ensure Children Receive Recommended Screenings
Fast Facts
Medicaid, which provides health care for low-income and medically needy people, has an early screening and treatment benefit to help young people get the health care services they need. Goals of the benefit include getting blood lead screenings for young children and well-child exams for at least 80% of eligible young people.
We found
59% of those eligible got at least one recommended exam in 2017
3 states met the 80% target
Data on blood lead screenings is incomplete, so nobody knows how many young children were screened. Our recommendations include improving lead screening data and evaluating state performance in meeting targets.
Percentage of Medicaid Beneficiaries Aged 20 and Under Receiving At Least One Recommended Well-Child Screening in Fiscal Year 2017, By State
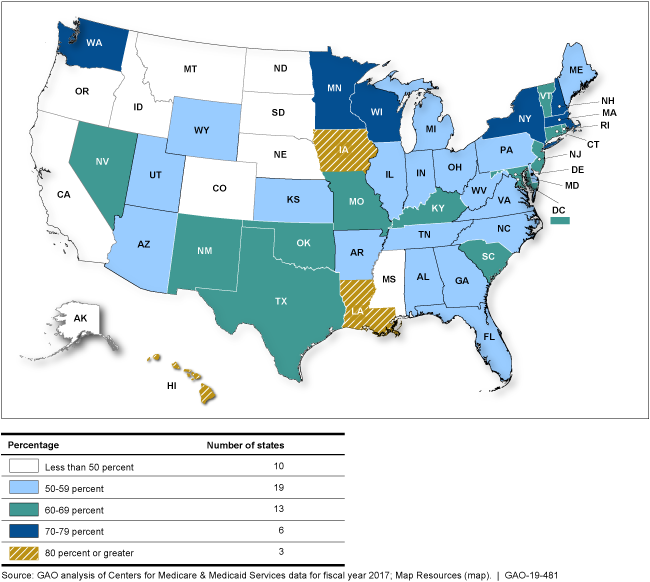
This map shows the percentage of beneficiaries receiving at least one recommended well-child screening in each state.
Highlights
What GAO Found
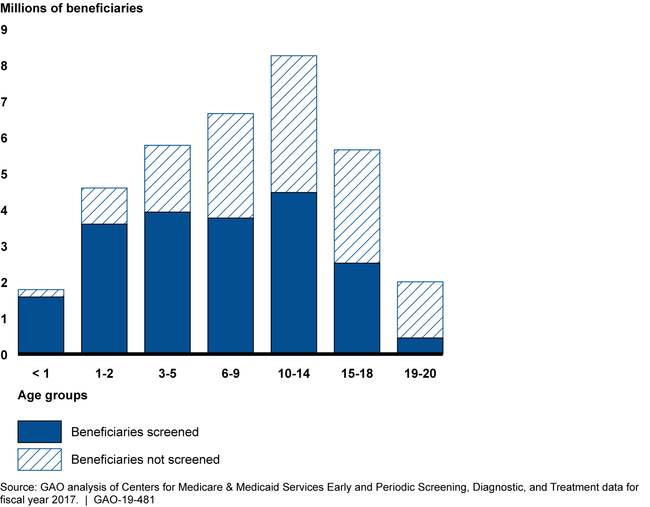
Approximately half of all Medicaid beneficiaries aged 20 and under received screenings and services recommended under the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit in fiscal year 2017, but nearly as many did not. For example, GAO's analysis of state-reported data found that about 59 percent of all beneficiaries (20.2 million) who should have received at least one recommended well-child screening received one. About 48 percent of beneficiaries aged 1 to 20 (18.3 million) received a preventive dental service in fiscal year 2017. Older beneficiaries tended to have lower rates of screening.
Number of Medicaid Beneficiaries Receiving and Not Receiving Well-Child Screenings in Fiscal Year 2017, by Age Group
The Centers for Medicare & Medicaid Services (CMS), the agency that oversees Medicaid, including EPSDT, has taken steps to improve the quality of information that states report about the provision of EPSDT services. CMS has also set some EPSDT performance measure targets for states; yet, the agency has not taken other steps to oversee the EPSDT benefit, such as
- collecting the data necessary to evaluate whether states are complying with CMS's policy for beneficiaries to receive a blood lead screening;
- taking action, as needed, based on assessments of the appropriateness of some performance measures, such as well-child screening measures; and
- using state-reported information to regularly evaluate states against CMS's EPSDT targets, or assisting states in planning improvements to meet the targets.
Absent these steps, CMS's oversight is limited and beneficiaries may not be receiving appropriate EPSDT services when they need them.
Why GAO Did This Study
The EPSDT benefit is key to ensuring that Medicaid beneficiaries aged 20 and under receive periodic screening services, such as well-child screenings, and diagnostic and treatment services, such as physical therapy and eyeglasses, to correct or ameliorate conditions discovered during a screening.
GAO was asked to examine the extent to which Medicaid beneficiaries aged 20 and under receive health care services under the EPSDT benefit. Among other things, GAO examined (1) what is known about the provision of EPSDT services based on CMS-required annual state reporting, and (2) CMS oversight of the EPSDT benefit. To do this, GAO analyzed annual state reporting data from fiscal years 2010 through 2017, the most current year data were available; CMS documentation; and federal internal control standards. GAO also interviewed CMS officials and Medicaid officials from 16 states selected, in part, on the variation in number of beneficiaries and geographic diversity.
Recommendations
GAO is making six recommendations to CMS regarding its oversight of the EPSDT benefit, including collecting appropriate blood lead screening data; taking action, if needed, after assessing the appropriateness of performance measures and targets for EPSDT; and evaluating states' performance in meeting CMS's EPSDT targets. CMS agreed with three recommendations, but disagreed with three others regarding performance measures and targets. GAO maintains that these recommendations are valid, as discussed in this report.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services |
Priority Rec.
The Administrator of CMS should work with states and relevant federal agencies to collect accurate and complete data on blood lead screening for Medicaid beneficiaries in order to ensure that CMS is able to monitor state compliance with its blood lead screening policy, and assist states with planning improvements to address states' compliance as needed. (Recommendation 1) |
As of February 2025, CMS stated that it continues to remind states of Medicaid's universal blood lead screening requirement and has encouraged state Medicaid agencies and health departments to continue undertaking additional efforts to increase these rates. In addition, CMS added a lead screening measure to the Child Core Set, which is a set of quality measures reported by states that is used, among other things, to monitor performance at the state level. States began reporting this measure in late 2023 and CMS expected these data to be available in late 2024. CMS also said it expects to release updated guidance on blood lead screening in 2025. CMS has previously said the updated guidance will emphasize the importance of complete and accurate data. These are positive steps that can assist CMS as it continues to consider how to help address known limitations in the current blood lead screening data, such as the under-counting of blood lead screening tests not paid for by Medicaid (and therefore which are not included in the current data). We will continue to monitor CMS's issuing of the guidance and update its status accordingly. To implement this recommendation, CMS should fully address limitations in blood lead screening data to better monitor compliance with the agency's blood lead screening policy.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should regularly assess the appropriateness of performance measures and targets for the EPSDT benefit, and take any necessary actions to ensure their relevance and use, including adding, changing, or removing measures, or targets, and regularly communicating performance measures and targets to states. (Recommendation 2) |
As of February 2025, CMS continued to report that the agency does not concur with this recommendation. CMS has previously noted this is in part because the agency does not have the authority to set binding targets for every EPSDT measure. As we stated in our report, our recommendation does not assume that targets should be set for every measure. GAO maintains that CMS needs to regularly assess the appropriateness of performance measures and targets for the EPSDT benefit and communicate them to states. This includes assessments of the CMS-416 performance measures, such as the participant and screening ratios, which CMS officials acknowledge have limitations.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should conduct regular evaluations of state performance by comparing states' performance measurement data with CMS's EPSDT targets to identify gaps in states' performance and areas for improvement. (Recommendation 3) |
As of February 2025, CMS continued to report that the agency does not concur with this recommendation. CMS has previously noted this is in part because the agency provides states with information about their performance on ESPDT measures reported on the Child Core Set, including a state's performance relative to other states' performance. We noted the limitations of this approach in our report; descriptions of a state's performance relative to other states is subject to change over time. For example, because the median is the midpoint of all states' performance, it ensures that half of states will not meet it, regardless of their individual performance. GAO maintains that a fixed target--or targeted improvement goal, such as the one developed as part of the Oral Health Initiative--would provide states with the opportunity to measure performance over prior years' results, which is a more meaningful measure that all states can strive to achieve.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should assist states with planning needed improvements, including providing focused assistance, to resolve gaps in states' performance in meeting CMS's EPSDT targets. (Recommendation 4) |
As of February 2025, CMS continued to report that the agency does not concur with this recommendation. CMS has previously noted this is in part because the agency does not believe that it is productive or appropriate to set targets for every EPSDT measure. As we stated in our report, our recommendation does not assume that targets should be set for every measure. However, developing additional targets on performance measures critical to beneficiaries' health and well-being could help improve oversight of EPSDT. GAO maintains that targeted technical assistance could be valuable for CMS to provide to states after identifying gaps in states' performance relative to EPSDT targets. Doing so would allow CMS to share additional strategies to help states plan and implement needed improvements.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should develop a plan with time frames and interim milestones for using T-MSIS data to generate the necessary data from the CMS-416 to improve EPSDT oversight and streamline state reporting. (Recommendation 5) |
In June 2020, CMS officials reported that the CMS-416 has been updated to provide an option for states to allow CMS to complete the form on their behalf using T-MSIS data. States will begin to use this form in 2021 for the submission of FY 2020 data. According to the instructions for completing the CMS-416, this option is available to states that are current with T-MSIS data submissions and pass T-MSIS benchmarks for data quality and completeness. States that select this option will be given an opportunity to review and validate the T-MSIS generated report before it is finalized and made publicly available. States that choose not to have CMS generate the state-specific CMS-416 or that do not meet the criteria to have CMS generate the CMS-416 will continue to complete the CMS-416 themselves.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should develop a plan with time frames and interim milestones for using T-MSIS data to generate the necessary data from the Child Core Set to improve EPSDT oversight and streamline state reporting. (Recommendation 6) |
As of February 2025, CMS stated the agency continues to assess the feasibility of extracting Core Set data for select quality measures using T-MSIS data, in order to reduce the administrative burden on states. CMS previously stated that it was conducting a pilot to explore the feasibility of using T-MSIS data to generate certain Child Core Set measures. GAO will continue to follow the agency's progress on this activity.
|
