Health Care Quality: CMS Could More Effectively Ensure Its Quality Measurement Activities Promote Its Objectives
Fast Facts
How does Medicare ensure that hospitals, physicians, and others are providing high-quality health care?
Medicare can adjust payments based on performance, but it also keeps providers accountable by making health care quality information publicly available. Medicare has made it a priority to develop and use measures of health care quality that address key aspects of care while minimizing the data reporting burden on providers.
However, it isn’t always clear that Medicare’s measures address its priorities. We recommended ways to ensure Medicare’s priorities drive its quality measurement activities.

Stethoscope and a calculator on top of a medical bill
Highlights
What GAO Found
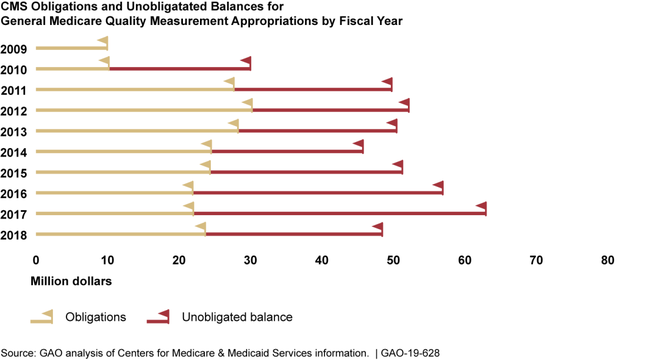
The Centers for Medicare & Medicaid Services (CMS), within the Department of Health and Human Services (HHS), maintains information on the amount of funding for activities to measure the quality of health care provided under Medicare. CMS's information shows it has carried over from each year to the next large amounts of available funding—known as unobligated balances—for quality measurement activities from fiscal years 2010 through 2018 (see figure). CMS officials said they maintained such available funding to ensure there were no gaps in funding for future years. However, CMS officials also told GAO that the information it maintains does not identify all of the funding the agency has obligated for quality measurement activities. Further, it does not identify the extent to which this funding has supported CMS's quality measurement strategic objectives, such as reducing the reporting burden placed on providers by CMS's quality measures. With more complete and detailed information, CMS could better assess how well its funding supports its quality measurement objectives.
CMS takes different approaches for deciding which quality measures to develop and to use. However, CMS lacks assurance that the quality measures it chooses address its quality measurement strategic objectives. This is because CMS does not have procedures to ensure systematic assessments of quality measures under consideration against each of its quality measurement strategic objectives, which increases the risk that the quality measures it selects will not help the agency achieve those objectives as effectively as possible. These procedures, such as using a tool or standard methodology to systematically assess each measure under consideration, could help CMS better achieve its objectives. In addition, CMS has not developed or implemented performance indicators for each of its quality measurement strategic objectives. Establishing these indicators and using them to evaluate its progress towards achieving its objectives would enable CMS to determine whether its quality measurement efforts are sufficient or changes are warranted.
Why GAO Did This Study
To encourage greater value in health care, CMS adjusts its Medicare payments to many health care providers based on measures of the quality of care. Therefore, the decisions CMS makes to choose certain quality measures have significant consequences. These decisions may involve selecting specific existing measures for CMS to use, stopping the use of some measures, or identifying new measures to be developed.
The Bipartisan Budget Act of 2018 contains a provision for GAO to review CMS's quality measurement activities. For this report, GAO (1) assessed the information CMS maintains on funding of health care quality measurement activities, and (2) described and assessed how CMS makes decisions to develop and to use quality measures. GAO analyzed CMS funding data for 2009 through 2018 and data on CMS quality measurement selections for 2014 through 2018. GAO reviewed CMS documentation related to its decisions on quality measurement and interviewed program and contractor officials.
Recommendations
GAO recommends that CMS (1) maintain more complete and detailed information on its funding for quality measurement activities, (2) establish procedures to systematically assess measures under consideration based on CMS's quality measurement strategic objectives, and (3) develop and use performance indicators to evaluate progress in achieving its objectives. HHS concurred with all three recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should, to the extent feasible, maintain more complete information on both the total amount of funding allocated for quality measurement activities and the extent to which this funding supports each of its quality measurement strategic objectives. (Recommendation 1) |
As of January 2025, CMS reported that it has implemented a new budget system that improves its ability to track how its budgetary allocations align with its quality strategic plan. According to CMS officials, this system allowed them to identify budgetary resources for quality measurement activities in a reasonable and accurate way. We are in the process of obtaining documentation from CMS to show the extent to which this system's implementation had allowed CMS to link funding amounts to activities in its quality strategic plan, as expected. Linking funding amounts in this way could provide CMS with better information on how its allocated resources relate to the quality measurement objections it is trying to achieve.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should develop and implement procedures to systematically assess the measures it is considering developing, using, or removing in terms of their impact on achieving CMS's strategic objectives and document its compliance with those procedures. (Recommendation 2) |
As of January 2025, CMS reported that, for some of its quality measure decisions, its Quality Measure Index (QMI) allows it to systematically assess the relative value of quality measures based on key measure characteristics, including the extent to which they address strategic objectives outlined in CMS's National Quality Strategy. Specifically, CMS uses the tool to help assess measures under consideration for use in CMS's various quality measurement programs. Regarding new measure development, CMS stated that it had used the QMI to test certain measures under development, which will facilitate future routine scoring of these measures. CMS also stated that it was refining the tool to score measures after the initial stage of development, which would inform decisions on whether to continue their development. Regarding decisions on which measures should be removed, CMS reported that it used the Consensus-Based Entity to develop a separate Measure Set Review process. However, CMS did not provide information on whether this process includes an assessment of the measures' contributions toward CMS's strategic goals. To fully implement this recommendation, CMS should share documentation showing how assessments of measures' impact on its strategic goals informed its decisions on measure development, use, and removal.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should develop and use a set of performance indicators to evaluate the agency's progress towards achieving its quality measurement strategic objectives. (Recommendation 3) |
As of January 2025, CMS's responses to this recommendation have focused on a series of impact assessments for quality measures, such as the 2021 National Impact Assessment of CMS Quality Measures Report. That report summarizes trends in the level of performance achieved on CMS's existing quality measures. However, this recommendation called on CMS to develop a separate set of performance indicators to assess the extent to which its quality measurement activities as a whole are achieving its strategic objectives for quality measurement, and to identify any gaps in meeting those goals. Such indicators would help CMS to make adjustments to its set of quality measures in order to more fully meet the strategic objectives it has established.
|
